Flatfoot is one of the most prevalent foot disorders. People with flat feet feel pain in their back, knees, and hips when walking and running. To mitigate this pain, researchers at Université de Montréal and Polytechnique Montréal are currently working to design, optimize, and manufacture a functional orthopedic trabecular insole, which will be released by the end of 2021.
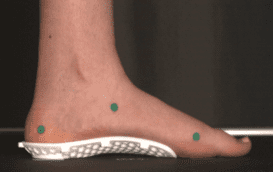
“3D printed, personalized insole for a patient with flat feet. This project is a collaboration between Polytechnique Montréal (LM2 lab), the Université de Montréal (S2M lab) and an industrial partner, Médicus.”
The medial longitudinal (inner) arch of the foot plays a significant role in body movement as it provides needed elasticity and shock absorption. A limited or a flexible longitudinal arch affects the walking function, especially ankle, knee, and hip joint alignment. Orthopedic insoles or foot orthotics represent one of the most common devices prescribed to mitigate the difficulties of such foot disorders. In this project, advanced 3D scanning techniques and 3D printing are used to produce customized orthopedic insoles to meet individual patient needs.
Design starts with foot topology. The insole’s initial geometry comes from a 3D scan of the patient’s foot. Next, the geometry of the lattice insole is optimized to provide variable mechanical properties to meet the therapeutic needs of individual patients with flat feet. The optimized insole is then manufactured by 3D printing. This technology makes it possible to design and build foot orthotics with complex geometry for specific patients affordably.
Yet, determining the therapeutic needs of a specific patient with flat feet is challenging, due mainly to individual variability in foot shape and gait biomechanics. In fact, flatfoot includes a broad spectrum of clinical pathologies; researchers in biomechanics are still trying to understand the causes and develop solutions. Many clinical tests are required to identify each patient’s specific needs, find an appropriate therapy, and correspondingly, design and manufacture an orthopedic insole.
My project, currently underway, paves the way to simulating and predicting the foot and insole’s mechanical response, which helps identify specific patients’ therapeutic needs. To this end, three-dimensional surface scanning technologies provide accurate digital representation of foot topology. Magnetic resonance imaging (MRI) serves to accurately depict the shape or geometry of internal foot features (e.g. bones, soft tissues, ligaments). A computer simulation of the foot and insole can then be generated by using the geometric depiction and assuming approximate mechanical properties of each feature.
The finite element method (FEM), a mathematical problem-solving method, is used next to analyze the biological system. FEM finds the mechanical response of a structure under given loading and boundary conditions. But finite element simulation is a demanding task when it comes to such a complicated biological system, even with modern computers. To design and optimize an insole for each patient, simulations must be run many times. Thus, there is a need for a fast and computationally efficient model to help orthotists design customized and optimal insoles.
My first objective is to design a surrogate model that is computationally efficient and equivalent to the large-scale and detailed simulation. The surrogate, therefore, should provide approximately the same response when compared to the original model. Replacing the sophisticated and detailed simulation with the surrogate will help significantly reduce the computational time, for instance, from two hours to only a few seconds.
But, no matter how fast the model, its predictions need to be validated by real-world observations. In fact, predictions from both the detailed and surrogate models should correspond to experimental measurements taken during dynamic loading (walking) and static loading (standing position). Consequently, my second objective is to compare the computational results to the experimental measurements for validation. I am still in this difficult validation stage. Once the models have been validated, they can be used to optimize insoles.

The question remains: what is the target function in our optimization? For now, this is still unknown. There is no mathematical function to optimize and find the best insole for a patient. However, I can run the simulation for a patient with a given insole and evaluate outputs such as foot deformation or pressure distribution over the insole to assess its performance. Thus, I can generate simulations using some 100,000 insoles of varying geometrical parameters for a patient and, in light of the biomechanical response, I can comparatively select the best one. The 3D printed optimized orthopedic insole should then allow patients to walk and run comfortably in their daily lives.
This article was produced by Mohammad Reza Moeini Gharagozlo, PhD (third year), Mechanical engineering department (Polytechnique Montreal), with the guidance of Marie-Paule Primeau, science communication advisor, as part of our “My research project in 800 words” initiative.